
Report #5: Getting an Autism Diagnosis and Follow-Up Care
A Survey of Individuals and Families Living with Autism
About the Autism Needs Assessment
The Bureau of Autism Services, in its effort to improve care and quality of life for Pennsylvanians with autism and their families, conducted the PA Autism Needs Assessment. This effort has been a key task of the ASERT (Autism Services, Education, Resources and Training) Collaborative and has been led by University of Pennsylvania School of Medicine, Center for Mental Health Policy and Services Research and the Center for Autism Research at The Children’s Hospital of Philadelphia.
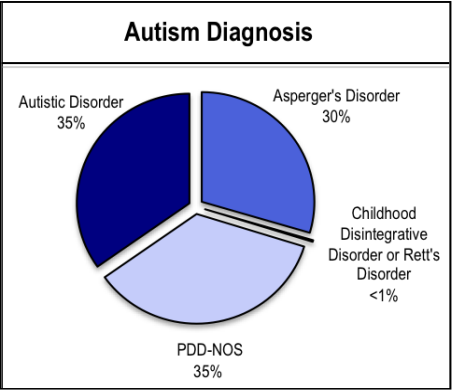
Autism Spectrum Disorders (ASD), referred to as autism throughout these reports, include Autistic Disorder, PDD-NOS, Asperger’s Disorder, Childhood Disintegrative Disorder and Rett’s Disorder. With more than 3,500 responses, the survey is the largest of its type to date in the nation. The findings from this needs assessment highlight challenges that Pennsylvanians with autism, of all ages, face everyday.
This report is the fifth in a series. The recommendations in this report address diagnosis and follow-up care among Pennsylvanians living with autism.
Why Examine Autism Diagnosis and Follow-Up Care?
Community awareness of autism has increased exponentially in the last two decades. As a result, caregivers notice developmental delays earlier and professionals diagnose autism in children at a younger age. Even so, diagnosis and follow-up care is still a long and difficult process. Receiving a diagnosis and services earlier in life results in better outcomes. This report addresses the process of getting an autism diagnosis and follow-up care in Pennsylvania. Understanding the challenges that individuals and families face in receiving an autism diagnosis and connecting with follow-up care is important in guiding changes to policy and practice. This report concludes with specific recommendations to ensure early diagnosis and appropriate follow-up care.
Shown below are the percentages of survey respondents with each specific autism diagnosis.
Diagnosis & Follow-Up Care
Age of First Concern
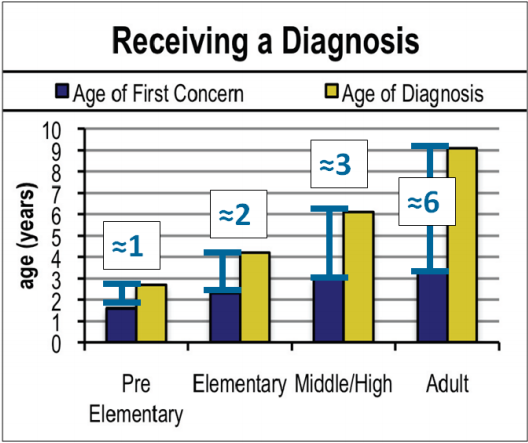
- The average age of diagnosis is getting younger over time. Increased awareness of autism has helped parents of younger children recognize the signs of autism an average of 2 years earlier than did parents of individuals who are now adults.
- Adults who were diagnosed prior to the current increase in autism awareness experienced more obstacles and delays in obtaining an autism diagnosis than younger children diagnosed more recently.
- There is a six-year difference between the age when individuals in the adult group were diagnosed and the age when individuals in the pre-elementary group were diagnosed.
- The gap between first concern about development and age of diagnosis has decreased over time.
- However, even for the most recently diagnosed children, there was a gap of more than a year from when a caregiver first noticed a delay in development until their child received an autism diagnosis
Prior Diagnoses
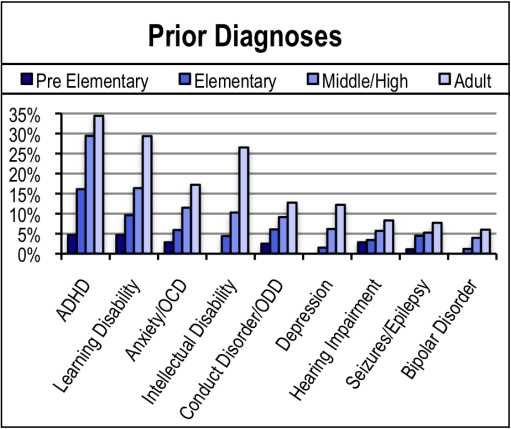
- Close to 60% of caregivers of individuals with autism indicate that their child had been diagnosed with another disorder prior to being diagnosed with autism.
- In some cases, the prior diagnosis may act as a gateway to further assessment, leading to the autism diagnosis.
- Adults were most likely to have received multiple prior diagnoses before receiving an autism diagnosis.
Number of Professionals Seen and Distance Traveled to Obtain Diagnosis
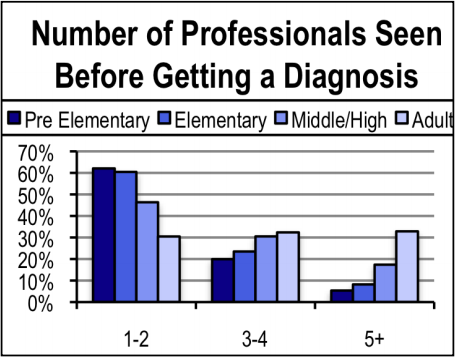
- Increased autism awareness has improved the ability of professionals to accurately diagnose autism. Most (60%) younger children with autism were diagnosed after visiting only 1 or 2 professionals, but most adults with autism (65%) saw three or more professionals before receiving a diagnosis.
- Caregivers in rural areas traveled farther than caregivers in urban counties to receive an autism diagnosis.
Follow-Up Services
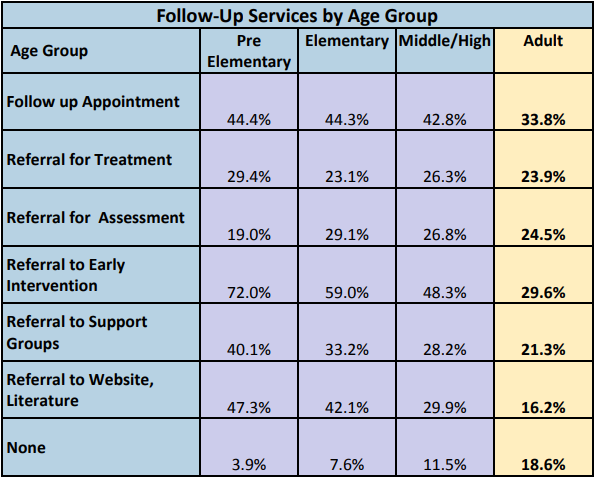
- Referrals to follow-up services post-diagnosis have increased over time. Still, less than half of families of pre-elementary school children are referred to treatment or follow-up appointments.
- Caregivers of adults consistently report fewer referrals to follow-up services than other age groups, with almost 19% reporting no referrals at all. Certain services, such as websites, literature and support groups, may not have been available when adults with autism were first diagnosed.
Recommendations
1. Expand the capacity to provide appropriate diagnosis and assessment of children and adults with autism.
Accurately diagnosing children and adults with autism is a highly specialized skill. Much of the delay in diagnosing individuals with autism is due to the lack of geographically accessible, qualified professionals with this specialized skill set. Diagnosing an individual with autism also requires more time and interaction between professionals from different backgrounds and areas of expertise than a typical doctor’s office visit allows.
Targeted autism-specific training, combined with ongoing consultation with experienced professionals, is needed in order to increase the capacity for accurate and timely diagnosis. In order to decrease wait and travel time, priority should be placed on providing resources and training to practitioners supporting rural and other underserved areas. Developing incentives and a means for multiple practitioners to coordinate assessment is also important to ensure an accurate diagnosis
2. Develop regional databases of services and supports that families can use to learn about places to obtain accurate diagnosis, and that families and clinicians can use to refer to and access appropriate follow-up services.
Families and individuals need support after receiving an autism diagnosis. They need to be easily connected to available, reputable, and effective services, specialists, support groups and information to guide care. Services often are fragmented, however, and there often is little information available about where and how to access these services. Regularly-maintained databases that provide this information should be developed. This information should be available on-line and also in print form in doctors’ offices, libraries and other high-traffic areas.
